MINUTES MATTER
Faster is Better in Hemorrhage Control
Time to hemorrhage control is critical when minutes mean blood loss.
Time to hemorrhage control is critical when minutes mean blood loss.
Every effort should be made to decrease the time to administration of the first blood products.1
Each minute of delay between the activation on an MTP and the arrival of the first blood products results in a 5% increase in the odds of mortality.1
Timely delivery of blood products is an important metric, similar to “door-to-balloon” time.1
Early Fibrinogen Supplementation Improves Patient Outcomes*
Early delivery of fibrinogen and other vital clotting factors add the clotting strength needed to achieve stable clot formation and restore hemostasis.2,3
Reduces blood component utilization4,5,6
Lowers mortality4
Shortens ICU stay and overall length of stay5
Decreases surgical procedures & wound infection5,6
Massive Transfusion Protocols (MTP) improve hemorrhage outcomes by delivering blood products quickly, but they lack critical components from the start.
In today’s MTP’s, sources of clotting factors (e.g. cryopreciptated Antihemophillic Factor (cryo AHF)) for the treatment of coagulaopathy in hemorrhage often arrive too late to be medically efficacious.7,8
MTPs Lack Critical Components from the Start
Cryoprecipitated AHF Inventory Challenges

>75%
In >75% of U.S. exsanguination cases, cryo AHF arrives too late to be medically efficacious.7,8†
Delays Impact Cryoprecipitated AHF Utility
Time to issue cryo AHF by patient type12*
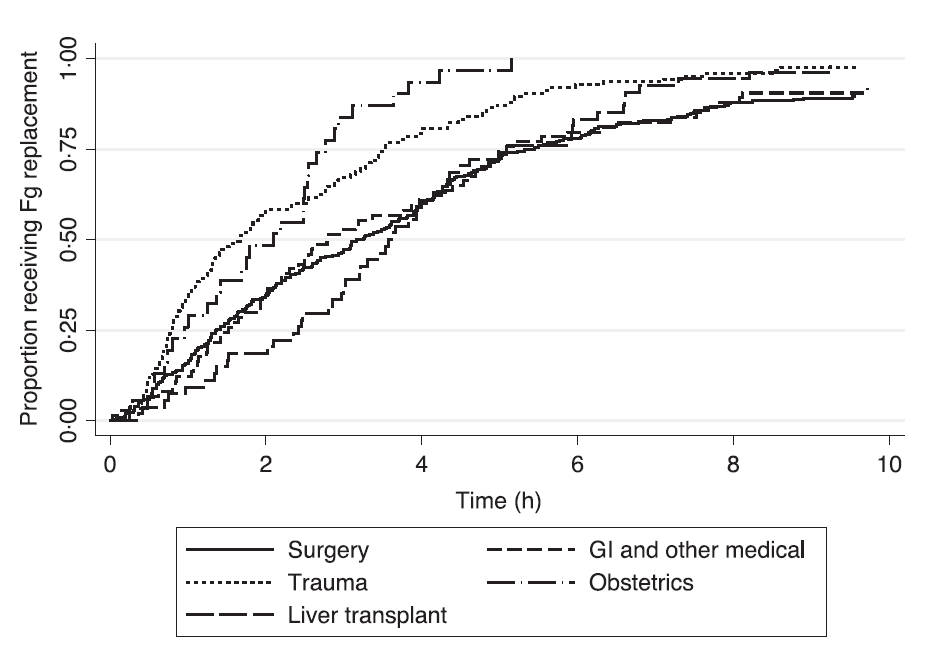
* ©2017 John Wiley & Sons Ltd. Graph reproduced with permission.
- 2.5 hours: Median time to receipt of cryo AHF after initiation of an MTP12
- Trauma and OB earliest: median of 1.7 hours12
- 1.6 hours: Median time to death from exsanguination7
Improving fibrinogen levels earlier may help close the mortality gap13,14
Be Ready.
When Minutes Matter®
You may also be interested in
†Data on file
References:
- Meyer DE, et al. Every minute counts: Time to delivery of initial massive transfusion cooler and its impact on mortality. The journal of trauma and acute care surgery 2017;83:19-24.
- Rourke C, et al. Fibrinogen levels during trauma hemorrhage, response to replacement therapy, and association with patient outcomes. Journal of thrombosis and haemostasis. JTH 2012;10:1342-51.
- Levy JH, et al. Fibrinogen and hemostasis: a primary hemostatic target for the management of acquired bleeding. Anesthesia and analgesia 2012;114:261-74.
- Ditillo M, et al. The role of cryoprecipitate in massively transfused patients: Results from the Trauma Quality Improvement Program database may change your mind. J Trauma Acute Care Surg, 2020. 89(2): p. 336-343.
- Pearse BL, et al. Protocol guided bleeding management improves cardiac surgery patient outcomes. Vox Sang, 2015. 109(3): p. 267-79.
- Green L, et al. Early cryoprecipitate transfusion versus standard care in severe postpartum haemorrhage: a pilot cluster-randomised trial. Anaesthesia, 2022. 77(2): p. 175-184.
- Cripps MW, et al. Cause and timing of death in massively transfused trauma patients. The journal of trauma and acute care surgery 2013;75:S255-62.
- Holcomb JB, et al. Cryoprecipitate Use in the Prospective Observational Multicenter Major Trauma Transfusion study (PROMMTT). The journal of trauma and acute care surgery 2013;75:S31-S39.
- AABB. Circular of Information for the Use of Human Blood and Blood Components. Bethesda, MD: AABB; 2021.
- Dunbar NM, et al. Blood component transfusion and wastage rates in the setting of massive transfusion in three regional trauma centers. Transfusion 2017;57:45-52.
- Wagner SJ, et al. Bacterial safety of extended room temperature storage of thawed cryoprecipitate. Transfusion 2019;59:3549-50.
- McQuilten ZK, et al. Fibrinogen concentration and use of fibrinogen supplementation with cryoprecipitate in patients with critical bleeding receiving massive transfusion: a bi-national cohort study. Br J Haematol. 2017 Oct;179(1):131-141.
- Hagemo JS, et al. Prevalence, predictors and outcome of hypofibrinogenaemia in trauma: a multicentre observational study. Critical care 2014;18:R52.
- Morrison JJ, et al. Association of cryoprecipitate and tranexamic acid with improved survival following wartime injury: findings from the MATTERs II Study. JAMA surgery 2013;148:218-25.


